5 Prenatal Yoga Poses To Stop Pregnancy Aches and Pains
Here are things you can do to reduce your discomfort. Read more
Here are things you can do to reduce your discomfort. Read more
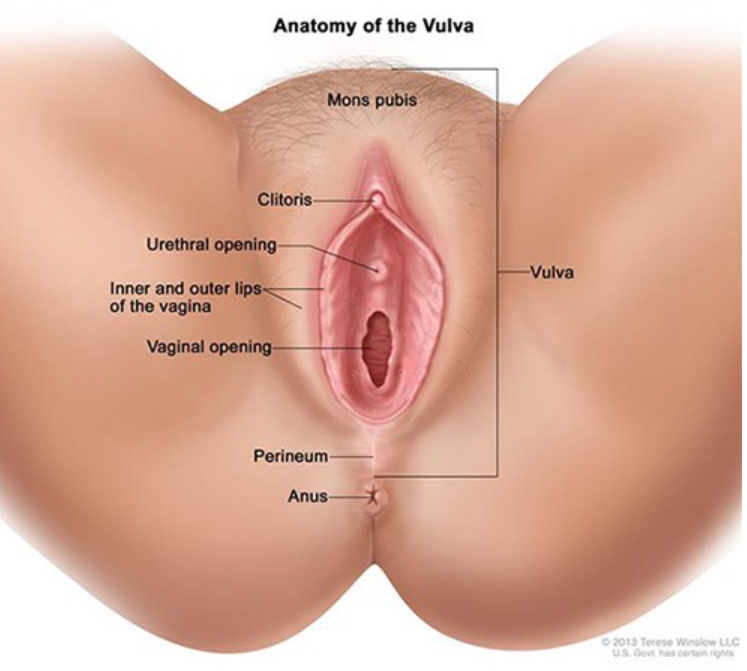
How to fix odor “down there”.
Let’s face it. Humans sometimes stink. Our genitals, butts, and armpits do not always smell like roses. Women expect postworkout smelly armpits, but no one is happy when the pungent odor comes from the vagina.
So, what causes the “not so fresh” feeling?
Sweat, food intake, medications, and hormonal changes all alter vaginal scent, but the most common cause of an unpleasant vaginal odor is an overgrowth of normal vaginal bacteria called bacterial vaginosis.
Bacterial vaginosis is easy to treat with antibiotics, but the crucial step is to confirm the diagnosis with a medical provider. Self-diagnosing often leads to errors. The malodorous situation “down there” will not improve if we are not treating the right thing.
While most women will get bacterial vaginosis at some point in their life, everyone wants to know why BV happens and how to get rid of it.
Bacterial vaginosis (BV) is not an infection in the traditional sense, but rather a condition caused by an overgrowth of anaerobic bacteria living in the vagina.
Vaginal bacteria are supposed to be present. Bacteria live on our skin, mouths, and gastrointestinal tracts all the time. These healthy bacteria help keep our body systems running smoothly. The vagina always contains small amounts of healthy, protective bacteria.
Vaginal bacteria and yeast live in perfect harmony, maintaining the vaginal ecosystem. Bacteria and yeast work to keep the vaginal chemistry pH balanced in the healthy range between 3.5–5.5.
Periodically, something disruptive happens to break the chemical balance allowing bacteria to flourish. When bacteria outgrows the counterbalancing yeast, women develop bacterial vaginosis.
When vaginal bacteria overpower and suppress yeast, women will notice a gray or yellow, fishy smelling discharge.
BV is the most common vaginal condition, and any woman can get it. BV is more common in sexually active women, but it is not a sexually transmitted infection.
BV is most common in ages 15 to 44, but it can happen at any age and in women who do not have sex.
The risk of bacterial vaginosis increases with:
BV symptoms vary from person to person. While some may have no symptoms, others will notice a fishy vaginal odor, vulvar irritation, or discomfort with urination. Some experience a watery or foamy white, yellow, or gray vaginal discharge.
These symptoms are often confused with STIs and vaginal yeast infections. Seeing your doctor or practitioner is the only way to determine if you have a BV and not a more severe problem.
The signs and symptoms of a BV are similar to other more serious infections. Trichomoniasis is a common STI that also causes itching and vaginal odor.
If left untreated, STIs and BV raise your risk of getting other STIs, including HIV. Untreated gonorrhea and chlamydia can lead to problems getting pregnant. BV can also lead to problems during pregnancy, such as preterm labor and premature delivery.
A doctor will do a pelvic exam to look for the characteristic discharge. The doctor may also use a cotton swab to take a sample of the discharge from the vagina.
A test can be done to see if the pH is elevated. The providers may add a chemical called KOH to perform a Whiff test. (Yes, this involves smelling the discharge). Finally, the provider may look at the sample under a microscope to evaluate for a particular finding called clue cells.
Nucleic acid amplification microbial testing is a widely available rapid test technology to help distinguish between yeast, bacterial vaginosis, and trichomoniasis.
BV is treated with prescription antibiotics. Metronidazole pills or vaginal gel are the most common. Clindamycin is a common acceptable alternative.
Sex partners do not need to be treated.
Patients suffering from recurrent bacterial vaginosis may qualify for more robust treatment protocols.
Many times, BV will resolve on its own. Vaginas are very effective at self-correcting. Untreated BV increases the risk of getting HIV, genital herpes, gonorrhea, chlamydia, and pelvic inflammatory disease. Women with HIV who get BV are also more likely to pass HIV to a male sexual partner.
The medicine used to treat BV is safe for pregnant women at any stage of pregnancy. All pregnant women with symptoms of BV should be tested and treated. Some evidence indicates a link between BV and preterm birth.
Researchers do not know exactly what causes BV, but we know ways to help the vagina maintain a normal pH and reduce the risk of BV. Steps include:
Thank you Sexography for publishing this article on Medium. Article originally published on Medika Life.
Blog Author: Dr. Jeff Livingston
Main Blog Photo By: Giulio_Fornasar stock by Getty
An OB-GYN reviews the early research and the protective role of the placenta.
Giving birth in a pandemic considerably ups the stakes of concern. Pregnant women around the world are worried they will catch Covid-19 and pass it on to their newborn baby. And we know that viral infections in pregnancy and postpartum can lead to poor outcomes in babies.
Much remains unknown about the coronavirus’s effects on pregnant women and babies, but a recent prepublished manuscript titled “Infant Outcomes Following Maternal Infection With SARS-CoV-2” demonstrates highly encouraging results.
The new data shows that babies born to women with Covid-19 demonstrate no increase in low birth weight, difficulty breathing, apnea, or respiratory infections through the first eight weeks of life.
Based on what scientists know right now, there is no evidence indicating pregnant women are more at risk of contracting Covid-19 than the general public, public, but they are at a higher risk of getting sick from the virus.
During pregnancy, women have a temporarily suppressed immune system and physiologic changes in their lung function. These changes put pregnant women at a higher risk of respiratory problems when they contract similar viruses, such as influenza or pneumonia. OB-GYNs therefore consider pregnant women to be an at-risk group for respiratory compromise if they contract Covid-19. Additionally, preterm labor is a known risk when pregnant women contract viral illnesses such as MERS, SARS, and influenza. Preterm labor most likely results from the severity of the maternal illness and is not directly linked to the virus itself. In other words, preterm labor is not simply a result of contracting these viruses but rather dependent on the degree of illness that results.
In addition to preterm labor, OB-GYNs are concerned about a pregnant woman’s potential to pass Covid-19 to her baby during gestation. This is an example of what doctors call vertical transmission. Fortunately, data surveillance so far indicates that in utero coronavirus infections are very rare. According to the American College of Obstetricians and Gynecologists July practice advisory, “the data are reassuring that vertical transmission appears to be uncommon.”
The new data shows that babies born to women with Covid-19 demonstrate no increase in low birth weight, difficulty breathing, apnea, or respiratory infections through the first eight weeks of life.
NIH research indicates that in utero mom-to-baby transmission is rare because the placenta is missing key components the virus needs to enter the fetal circulation, namely ACE2 receptors and the TMPRSS2 enzyme. Both the ACE2 receptor and TMPRSS2 are present in the placenta but only in tiny amounts. The low levels likely explain why SARS-CoV-2 is unlikely to cross the placenta from mom to baby.
Over the past few months, scientists have studied more than 1,500 cases of maternal coronavirus infections. Current management guidelines for infants born to mothers with SARS-CoV-2 are based on data from the National Registry for Surveillance and Epidemiology of Perinatal Covid-19 Infection.
Current guidelines are based on data from previous experience with maternal respiratory infections, such as SARS and MERS, combined with incoming studies on Covid-19. The PRIORITY study (Pregnancy Coronavirus Outcomes Registry), a collaborative project between researchers at UCSF and UCLA, is an ongoing effort to track outcomes of pregnant women who contract SARS-CoV-2. This data surveillance adds valuable additional infant-outcome data beyond the neonatal period to better inform management policies and guidelines.
The PRIORITY study’s first publication brings some encouraging and reassuring news to the medical community. Data indicates that infants born to Covid-19-positive mothers do well in the first six to eight weeks after birth.
The manuscript, accepted for publication in Clinical Infectious Diseases, reports the infant outcomes of 179 pregnancies complicated by Covid-19 infection compared to a control group of 84 Covid-19-negative gestations.
The PRIORITY study data showed no increase in preterm birth, NICU admission, or upper-respiratory infections. The study cohort yielded no pneumonia or lower-respiratory infection cases through the first eight weeks of life.
The babies born to mothers with Covid-19 also showed a very low rate of acquiring the infection. Only 1.1% of infants tested positive in the first six to eight weeks when born to a mother who had Covid-19, confirmed by a positive SARS-CoV-2 PCR test. The Covid-19-positive infants demonstrated minimal symptoms.
The study authors note the limitations of the paper and encourage further studies to confirm newborn incidence rates, as they “were unable to estimate the incidence of infant SARS-CoV-2 infection because infant testing was incomplete and might be biased by both false-positive and false-negative results.”
The PRIORITY study’s control group includes both symptomatic and asymptomatic women who tested positive for SARS-CoV-2. The researchers indicate this cohort may not be representative of all U.S. pregnancies. The authors also note an underrepresentation of Black and LatinX moms in the study cohort compared to the current CDC statistics of pregnant women infected with SARS-CoV-2.
To improve future study participation, PRIORITY launched a Reproductive Health Equity and Birth Justice Core to increase enrollment of underrepresented groups.
Finally, the authors note that infant admissions to the NICU were higher among infants born to Covid-19-positive moms, and the babies were born at an earlier gestational age. The study authors were unable to determine if the increase in NICU admissions was directly related to SARS-CoV-2 or if the hospital practices for the management of mothers testing positive for Covid-19 explain the difference.
Thank you to Elemental for publishing this article on Medium.
Blog Author: Dr. Jeff Livingston
Main Blog Photo By: Carolyn Cole/Los Angeles Times/Getty Images
Endometrial polyps are a common cause of abnormal uterine bleeding. Read more
Improving maternal vaccination rates saves lives. Read more
Are you willing to perform beyond expectations? Read more
