Understanding how endometriosis affects your health and future pregnancy.
What is the deal with painful periods? Some people suffer every month while others never experience cramps. The most common cause of painful periods (dysmenorrhea) is endometriosis.
Endometriosis happens when tissue similar to the lining of the uterus grows outside of the uterus where it does not belong. It causes painful periods and affects more than 11% of American women. It is especially common among women age 25–35, and may impact ones ability to get pregnant. Several different treatment options can help manage the symptoms, improve your life, reduce pain, and improve your chances of getting pregnant.
What is endometriosis?
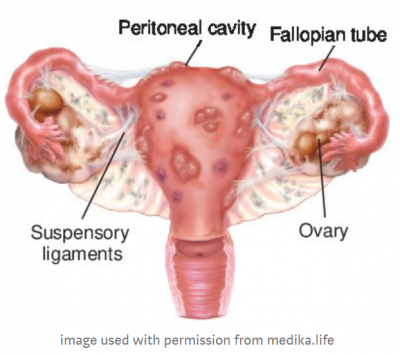
Endometriosis, sometimes called “endo,” is a common gynecologic health problem. It gets its name from the word endometrium, the tissue present in the lining of the uterus or womb. For women with endometriosis, this tissue begins growing outside of the uterus and on other areas in the body where it doesn’t belong.
Most often, endometriosis is found on the:
- Ovaries
- Fallopian tubes
- Tissues that hold the uterus in place
- The outer surface of the uterus
Endometriosis implants may also be found in the vagina, cervix, vulva, bowel, bladder, or rectum. Rarely, endometriosis appears in other parts of the body, such as the lungs, brain, and skin.
What are the symptoms of endometriosis?
Symptoms of endometriosis can include:
- Pain. Pelvic pain and painful periods are the most common symptoms. Women with endometriosis may have many different kinds of pain. These include:
- Very painful menstrual cramps (dysmenorrhea). The pain may get worse over time.
- Chronic (long-term) pain in the lower back and pelvis.
- Pain during or after sex (dyspareunia). Most endometriosis patients describe a “deep” pain distinctly different from discomfort at the entrance to the vagina during penetration.
- Bleeding or spotting between menstrual periods (metrorrhagia). Abnormal uterine bleeding has many causes and should be evaluated by your doctor.
- Infertility, or not being able to get pregnant.
- Stomach (digestive) problems. These include diarrhea, constipation, bloating, or nausea, especially during menstrual periods.
Why does endometriosis cause pain and health problems?
Endometriosis growths are benign (not cancerous), but they can still cause troublesome problems.
Remember, endometriosis implants occur when tissue similar to the lining of the uterus begins to grow outside of your uterus where it doesn’t belong. Endometriosis growths may swell and bleed in the same way the lining inside of the uterus does every month during menstrual cycles. This process causes swelling, pain, and scar tissue because the tissue grows and bleeds in an area where it cannot easily get out of your body.
The endometriosis implants may also continue to expand causing problems such as:
- Blocking the fallopian tubes.
- Benign ovarian tumors (endometriomas)
- Inflammation (swelling)
- Forming scar tissue and adhesions (a type of tissue that can bind your organs together).
- Problems in your intestines and bladder
How common is endometriosis?
Endometriosis is a common health problem for women affecting approximately 11% of women, or more than 6 ½ million women in the United States, have endometriosis. The exact number is unknown as many women who have endometriosis suffer no symptoms at all. Obgyns often discover endometriosis during routine surgeries such as tubal ligations.
Who gets endometriosis?
Endometriosis can happen to any woman who has menstrual periods, but it is more common in women 25–35 years old. Occasionally, we find endometriosis in young girls before they begin having periods which is called premenarcheal endometriosis.
You might be more likely to get endometriosis if you have:
- Never had children
- Menstrual periods that last more than seven days
- Short menstrual cycles (27 days or fewer)
- A family member (mother, aunt, sister) with endometriosis
- A health problem that blocks the normal flow of menstrual blood from your body during your period
What causes endometriosis?
No one knows for sure what causes this disease. Researchers are studying possible causes:
- Problems with the menstrual period flow. Retrograde menstrual flow is the most likely cause of endometriosis. Some of the tissue shed during the period flows through the fallopian tube into other areas of the body, such as the pelvis.
- Genetic factors. Because endometriosis runs in families, it may be inherited in the genes.
- Immune system problems. A faulty immune system may fail to find and destroy endometrial tissue growing outside of the uterus. Immune system disorders and certain cancers are more common in women with endometriosis.
- Hormones. The hormone estrogen appears to promote endometriosis. Research is looking at whether endometriosis is a problem with the body’s hormone system.
- Surgery. During abdominal surgery, such as a Cesarean (C-section) or hysterectomy, endometrial tissue can be picked up and transmitted to other areas of the body. For instance, endometrial tissue has been found in surgical scars.
How can I prevent endometriosis?
You can’t prevent endometriosis. But you can reduce your chances of developing it by lowering the levels of the hormone estrogen in your body. Estrogen helps to thicken the lining of your uterus during your menstrual cycle.
To keep lower estrogen levels in your body, you can:
- Talk to your doctor about hormonal birth control methods, such as pills, patches, or rings with lower doses of estrogen.
- Exercise regularly (more than 4 hours a week). This will also help you keep a low percentage of body fat. Regular exercise and a lower amount of body fat help decrease the amount of estrogen circulating through the body.
- Avoid large amounts of alcohol. Alcohol raises estrogen levels. No more than one drink per day is recommended for women who choose to drink alcohol.
- Avoid a large amount of caffeine. Studies show that drinking more than one caffeinated drink a day, especially sodas and green tea, can raise estrogen levels.
How is endometriosis diagnosed?
If you have symptoms of endometriosis, talk with your doctor. The doctor will talk to you about your symptoms and do or prescribe one or more of the following to find out if you have endometriosis:
- Pelvic exam. During a pelvic exam, your doctor will feel for large cysts or scars behind your uterus. Smaller areas of endometriosis are harder to feel.
- Imaging test. Your doctor may do an ultrasound to check for ovarian cysts from endometriosis. An ultrasound uses sound waves to create pictures of your reproductive organs.
- Magnetic resonance imaging (MRI) is another common imaging test that can take a picture of the inside of your body.
- Medicine. If your doctor does not find signs of an ovarian cyst during an ultrasound, he or she may prescribe medicine:
- Hormonal birth control can help lessen pelvic pain during your period.
- Gonadotropin-releasing hormone (GnRH) agonists block the menstrual cycle and lower the amount of estrogen your body makes. GnRH agonists also may help pelvic pain.
- If your pain gets better with hormonal medicine, you probably have endometriosis. But, these medicines work only as long as you take them. Once you stop taking them, your pain may come back.
- Laparoscopy. Laparoscopy is a type of surgery that doctors can use to look inside your pelvic area to see endometriosis tissue. Surgery is the only way to be sure you have endometriosis. Sometimes doctors can diagnose endometriosis just by seeing the growths. Other times, they need to take a small sample of tissue and study it under a microscope to confirm this.
How is endometriosis treated?
There is no cure for endometriosis, but treatments are available for the symptoms and problems it causes. Talk to your doctor about your treatment options.
Medication options
If you are not trying to get pregnant, hormonal birth control is generally the first step in treatment. This may include:
- Extended-cycle (you have only a few periods a year) or continuous cycle (you have no periods) birth control. These types of hormonal birth control are available in the pill or the shot and help stop bleeding and reduce or eliminate pain.
- Intrauterine device (IUD) to help reduce pain and bleeding. The hormonal IUD protects against pregnancy for up to 7 years. IUDs can reduce pain and bleeding.
The hormonal treatment works only as long as it is taken, and is best for women who do not have severe pain or symptoms.
Elagorix (brand named Orilissa) is a new medication indicated for endometriosis. It works by interacting with the hormones LH (luteinizing hormone) and FSH (follicle-stimulating hormone) to reduce the amount of circulating Estrogen. This medication is highly effective at reducing moderate to severe pain associated with endometriosis
If you are trying to get pregnant, your doctor may prescribe a gonadotropin-releasing hormone (GnRH) agonist. This medicine stops the body from making the hormones responsible for ovulation, the menstrual cycle, and the growth of endometriosis. This treatment causes a temporary menopause, but it also helps control the growth of endometriosis. Once you stop taking the medicine, your menstrual cycle returns, but you may have a better chance of getting pregnant.
Surgery
Surgery is usually chosen for severe symptoms, when hormones are not providing relief or if you are having fertility problems. During the operation, the surgeon can locate any areas of endometriosis and may burn, destroy, or remove the endometriosis implants. The surgeon may also test to see if the fallopian tubes are open (chromotubation). After surgery, hormone treatment is often restarted unless you are trying to get pregnant.
Other treatments you can try, alone or with any of the treatments listed above, include:
- Pain medicine. For mild symptoms, your doctor may suggest taking over-the-counter medicines for pain. These include ibuprofen (Advil and Motrin) or naproxen (Aleve).
- Complementary and alternative medicine (CAM) therapies. Some women report relief from pain with therapies such as acupuncture, chiropractic care, or supplements such as thiamine (vitamin B1), magnesium, or omega-3 fatty acids.
Does endometriosis go away after menopause?
For some women, the painful symptoms of endometriosis improve after menopause. As the body stops making the hormone estrogen, the growths shrink slowly. However, some women who take menopausal hormone therapy may still have symptoms of endometriosis.
If you are having symptoms of endometriosis after menopause, talk to your doctor about treatment options.
Can I get pregnant if I have endometriosis?
Yes. Many women with endometriosis get pregnant. But, you may find it harder to get pregnant. Researchers think endometriosis may affect as many as one in every two women with infertility.
No one knows exactly how endometriosis might cause infertility. Some possible reasons include:
- Patches of endometriosis block off or change the shape of the pelvis and reproductive organs. This can make it harder for the sperm to find the egg.
- The immune system, which normally helps defend the body against disease, attacks the embryo.
- The endometrium (the layer of the uterine lining where implantation happens) does not develop as it should.
If you have endometriosis and are having trouble getting pregnant, talk to your doctor. He or she can recommend treatments, such as surgery to remove the endometrial growths.
What other health conditions are linked to endometriosis?
Research shows a link between endometriosis and other health problems in women and their families. Some of these include:
- Allergies, asthma, and chemical sensitivities
- Autoimmune diseases, in which the body’s system that fights illness attacks itself instead. These can include multiple sclerosis, lupus, and some types of hypothyroidism.
- Chronic fatigue syndrome and fibromyalgia
- Certain cancers, such as ovarian and breast cancer
Thank you to BeingWell for publishing this article on Medium.
Article Originally published at https://medika.life on July 9, 2020.
Blog Author: Dr. Jeff Livingston
Main Blog Photo by: Anthony Tran on Unsplash