Our Preparing for series allows a patient to prepare themselves for a procedure properly. We answer questions about how long the procedure will last, what’s involved, what to expect, and even advice on packing your bag. While your surgeon preps, we’ll make sure you’re ready.
“Don’t make me laugh, cough, or sneeze.” For the one in four women over forty who suffer from stress urinary incontinence (SUI), one funny joke can lead to an embarrassing moment.
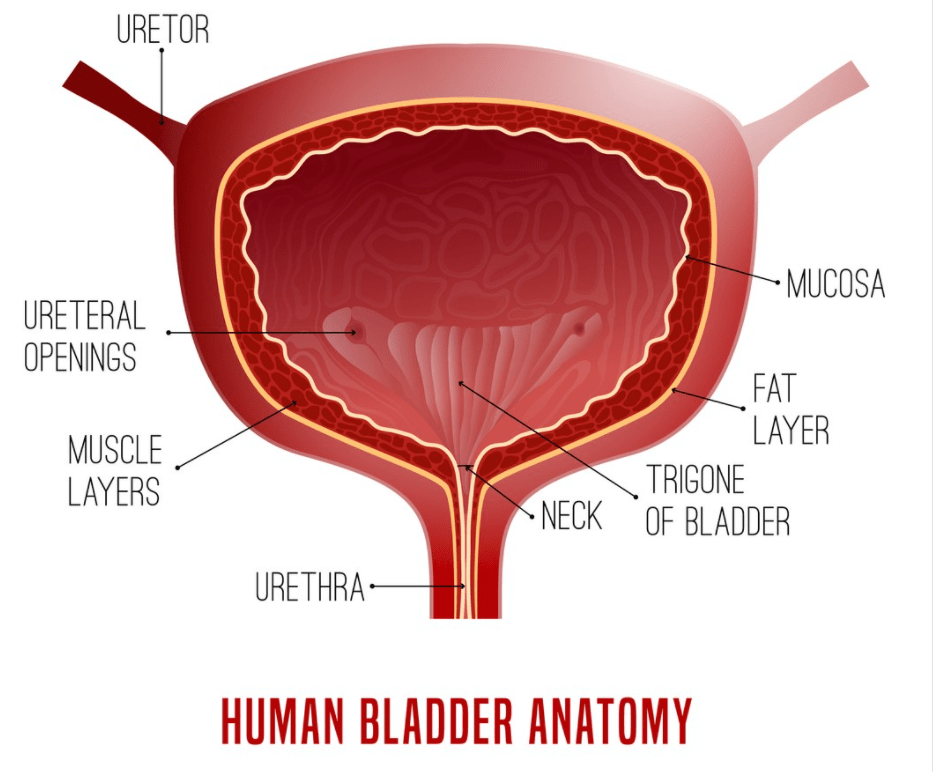
Stress urinary incontinence is the temporary loss of bladder control. SUI is triggered when bladder pressure overcomes the surrounding muscles designed to keep urine contained. Exercising, laughing, sneezing, or lifting heavy objects increases bladder pressure and can lead to accidents.
Stress urinary incontinence may be common, but it is never normal. No one has to live with bladder leaking.
Lifestyle changes improve symptoms. Overweight women often notice an improvement after weight loss. Reducing the intake of inflammatory chemicals like caffeine also helps. Eliminating smoking can decrease the number of times you leak.
Nonsurgical options such as pelvic muscle exercises and physical therapy can play a roll in the treatment of stress incontinence. Some women benefit from local injections of Botox or bulking agents like Collagen.
A minimally invasive surgical repair called a mid-urethral sling is an effective treatment to stop the leak,
Getting prepared for surgery can be scary. Learning about an upcoming procedure alleviates fear and anxiety. Let’s talk about a mid-urethral sling procedure and answer questions about how long it will last, what’s involved, what to expect, and even advice on packing your bag. While your surgeon preps, we’ll make sure you’re ready.
What is a Mid-urethral Sling?
A mid-urethral sling is the most common type of surgery used to correct SUI. A small, supportive material of synthetic mesh is placed under the bladder neck and then anchored to the other pelvic tissues creating a “hammock-like support” to prevent leakage.
The goal is to restore the natural support system for the bladder. These procedures are performed from a vaginal approach to minimizes incisions, pain, and recovery time. Mid-urethral slings are performed as outpatient surgery.
Photo By: fokusgood Istock by Getty
Where is a mid-urethral sling performed?
A mid-urethral sling can be performed in various settings, but most commonly, Obgyns performs this procedure in an Ambulatory Surgery center or hospital. Some Obgyns will do these surgeries in the office.
Choosing the appropriate surgical setting depends on a few different factors, including the physician’s experience, the availability of equipment impact the decision, and the extent of pelvic organ prolapse.
How long will I be in the hospital?
A mid-urethral sling is an outpatient procedure. Patients may go home after the surgery is complete. An overnight stay is not needed unless we are combining it with other gynecological surgeries.
Can my family visit me?
Most incontinence procedures are performed in a hospital or Ambulatory Surgery Center. A trusted family member should drive you to and from the appointment. Your family is welcome to stay with you before and after this outpatient procedure.
Does my procedure require an anesthetic?
Anesthesia is required for a mid-urethral sling procedure. The type of anesthesia will vary depending on the surgical setting, the surgeon’s experience, and office equipment availability.
Oral sedation, IV sedation, and general anesthesia are all potential anesthetic options. General anesthesia is the most common anesthetic choice for this type of surgery.
What’s the procedure when I check-in?
Most surgeries will involve a preoperative visit with your surgeon to go over the procedure’s risks and benefits in detail. Your surgeon answers questions regarding your upcoming surgery. The surgical consent form is reviewed, signed, or updated with any changes.
In most settings, patients will receive a preoperative phone call by a nurse or medical assistant one to two days before surgery. If any blood work or preoperative testing is required, it will be scheduled and confirmed.
The staff will guide you to the preoperative holding area to change into a surgical gown and store your valuables. You will meet the nursing team who will provide care during your stay. An IV will be placed at this time.
The anesthesia team will come to interview you and answer questions. Typically your surgeon will also come and review any last-minute questions.
What happens in the operating room?
After the preoperative evaluation, the team will guide you to the operating or procedure room. You will move from the mobile bed to the operating table. Once you are positioned comfortably and safely, the anesthesiologist will give you medication through your IV.
The OR nursing team will cover your body with sterile drapes and prep the vagina for surgical sterility. The team then performs a “surgical time-out.” A surgical safety checklist is read out loud requiring all surgical team members to be present and attentive.
The surgeon then performs the surgical procedure.
Once the procedure is complete, a post-procedure review is done together as a surgical team. All instruments and equipment are counted and verified. When finished, the anesthesiologist will begin to wake you up for transfer to the recovery room.
How does the procedure work?
Multiple medical device technologies can be used to perform mid-urethral sling surgeries. Urologists, urogynecologist, and gynecologic surgeons typically have a personal preference or comfort level with one or more of the various options.
Each medical device works similarly by providing support to the urethral to reduce the risk of stress incontinence. The entry point and attachment sites vary between different technologies.
The surgeon identifies the urethra and makes a small incision. The bladder is pushed away from the vaginal tissue to create a space. The synthetic mesh is placed under the bladder neck. The mesh is attached to the surrounding pelvic tissues to create support and prevent leakage.
The incisions are closed with sutures. Many surgeons examine the inside of the bladder with a camera to confirm no injuries occurred. This is called a cystoscopy.
Once the surgeon confirms, the bleeding is under control and the bladder is intact, then the procedure is complete.
What are the risks of a mid-urethral sling procedure?
The following risks are associated with any type of surgery for SUI:
- Injury to the bladder, bowel, blood vessels, or nerves
- Bleeding
- Infection of the urinary tract or wound infections
- Urinary retention (difficulty urinating or urgency symptoms)
- Problems related to the anesthesia
Synthetic mesh has a small risk of vaginal erosions when the mesh will erode through the vaginal tissue. Vaginal erosions are more common in patients with diabetes, obesity, and smokers. Additional surgery may be required to repair mesh erosion.
How long will I be in surgery?
Once the patient enters the operating room, a series of safety steps must occur. This process takes about 20 minutes.
The operative time for incontinence surgery varies if other gynecologic or urologic procedures are required.
In general, 30–60 minutes of total operative time should be expected.
When can I go home?
Postoperative recovery time will vary from person to person. Each patient must meet certain discharge criteria. The patient’s vital signs must be stable. The patient must be alert, oriented, and able to walk with assistance. Postoperative nausea, vomiting, and pain must be controlled as well as confirmation of no postoperative bleeding.
The nursing team will go over discharge instructions, and the plan for postoperative pain management options will be confirmed.
Mid-urethral sling procedures require a minimal amount of postoperative recovery. Patients are often discharged as early as 30–60 minutes after the procedure.
What is the usual recovery time
Most women should be able to return to normal daily activities within a few days. Patients will need to avoid heavy lifting or sexual activity until cleared by the doctor. Typically, the recommendation is no intercourse for 4–6 weeks
Some patients may notice difficulty starting the urine stream when trying to void. The tissue surrounding the urethra swells after surgery. This issue typically resolves quickly as the swelling subsides.
In rare cases, if a woman is not able to void, the stitches or the sling may need to be adjusted or removed.
Vaginal soreness and a small amount of bleeding are expected.
Some patients will require mild pain medication like NSAIDs or even low dose narcotics for a brief period of time.
It is wise to wear a sanitary pad for a few days as you may experience vaginal spotting or dark vaginal discharge.
What aftercare is required?
Most women should be able to return to normal daily activities and work within a few days.
After surgery, discomfort may last for a few days or weeks. During this time, avoid anything that puts stress on the surgical area, such as the following activities:
- Excessive straining
- Strenuous exercise
- Heavy lifting
- Sexual activity
Your doctor will schedule a postoperative examination 1–2 weeks after the procedure.
Danger Signals to look out for after the procedure
After a mid-urethral sling procedure, we expect light spotting and vaginal discharge.
If you experience heavy bleeding, abdominal or pelvic pain, a fever, or pain that increases over time beyond 24 hours, call your physician. After any surgery, contact your physician if you meet any of the following criteria:
- Pain not controlled with prescribed medication
- Fever > 101
- Inability to void (urinate)
- Nausea and vomiting
- Calf or leg pain
- Shortness of breath
- Heavy vaginal bleeding
- Foul-smelling vaginal discharge
- Abdominal pain not controlled by pain medication
- Inability to pass gas
What preparations should I make for aftercare at home?
Incontinence procedures require very little postoperative care. Vaginal discharge and spotting are expected. One should have a supply of sanitary pads available. Sexual activity should be avoided until cleared by your doctor. One may resume a normal diet and exercise the day after the procedure.
What information should I provide to my doctors and nurses?
It is very important to provide your doctor with an updated list of all medications, vitamins, and dietary supplements prior to surgery. All medication and food allergies should be reviewed. Share any lab work, radiologic procedures, or other medical tests done by other healthcare providers with your surgeon prior to your procedure.
Article originally published on Medika Life.
Blog Author: Dr. Jeff Livingston