Vaginal Hysterectomy; What You Need to Know and How to Prepare
An Obgyn explains this surgical procedure. Read more
An Obgyn explains this surgical procedure. Read more
An Obgyn explains this surgical procedure. Read more
We must have realistic vaccine expectations. Read more
Our Preparing for series allows a patient to prepare themselves for a procedure properly. We answer questions about how long the procedure will last, what’s involved, what to expect, and even advice on packing your bag. While your surgeon preps, we’ll make sure you’re ready.
A hysterectomy is a surgery to remove theuterus. Hysterectomies are performed for a variety of gynecologic conditions such as uterine fibroids, heavy periods, endometriosis, chronic pelvic pain, uterine prolapse and gynecologic cancer.
During a hysterectomy, the uterus is removed. Obgyns often recommend fallopian tube removal (bilateral salpingectomy) to reduce the risk of ovarian cancer. Some women will also need the removal of the ovaries (oophorectomy). Hormonal changes only occur when the ovaries are removed.
Gynecologists perform hysterectomies through a variety of techniques. The size of the uterus, surgeon experience, the patient’s body type, and the prior surgical history help determine the proper surgical approach. Techniques include:
Contrary to the name, robots do not perform the surgery. A human gynecologic surgeon attaches a surgical system to intraabdominal ports. While sitting at a surgical console, the surgeon controls the robotic arms while monitoring the surgical field in a 3D view..
Through 4–5 small incisions, the surgeon detaches the uterus from the surrounding tissues. Robotic surgery is a minimally invasive surgery that allows for faster recovery, reduced pain, and shorter hospital stay.
The American College of Obgyn acknowledges this type of hysterectomy’s growing popularity but recommends robotic hysterectomy be reserved for more complex cases that can not be safely completed through other minimally invasive techniques.
Experienced robotic surgeons prefer the precise control of the surgical arms allowing complex cases to be completed in a minimally invasive fashion. Patients benefit from small incisions, a short hospital stay, and a faster return to work, exercise, and everyday activities.
Surgeons perform robotic hysterectomies as an outpatient procedure or as an inpatient surgery with an overnight stay. Various factors, such as the patient’s underlying health status, surgical complexity, and physician preference, help determine the surgical plan.
Most robotic hysterectomy patients are able to leave the hospital much faster after a traditional abdominal hysterectomy.
A trusted family member should drive you to and from the hospital or ambulatory surgery center for a robotic hysterectomy. Families are welcome to stay with you before and after surgery. Hospital visitor policies for overnight stays vary from region to region due to the Covid-19 pandemic.
Laparoscopic robotic surgery requires general anesthesia meaning patients will be temporarily put to sleep. The surgeon may also inject a local anesthetic into the incisions to decrease postoperative pain.
Most surgeries will involve a preoperative visit with your surgeon to go over the procedure’s risks and benefits in detail. Your surgeon answers questions regarding your upcoming surgery. The surgical consent form is reviewed, signed, or updated with any changes.
Because robotic hysterectomies will eliminate the possibility of child-bearing, your doctor will ask questions to make sure you are confident you will not want children in the future.
In most settings, patients will receive a preoperative phone call by a nurse or medical assistant one to two days before surgery. If any blood work or preoperative testing is required, it will be scheduled and confirmed.
After arrival at the hospital or Ambulatory Surgery Center, the staff will guide you to the preoperative holding area to change into a surgical gown and store your valuables. You will meet the nursing team who will provide care during your stay. An IV will be placed at this time.
The anesthesia team will come to interview you and answer questions. Typically your surgeon will also come and review any last-minute questions.

After the preoperative evaluation, the team will guide you to the operating or procedure room. You will move from the mobile bed to the operating table. Once you are positioned comfortably and safely, the anesthesiologist will give you medication through your IV to help you go to sleep.
The OR nursing team will cover your body with sterile drapes and prep the abdomen for surgical sterility. The team then performs a “surgical time-out.” A surgical safety checklist is read aloud, requiring all surgical team members to be present and attentive.
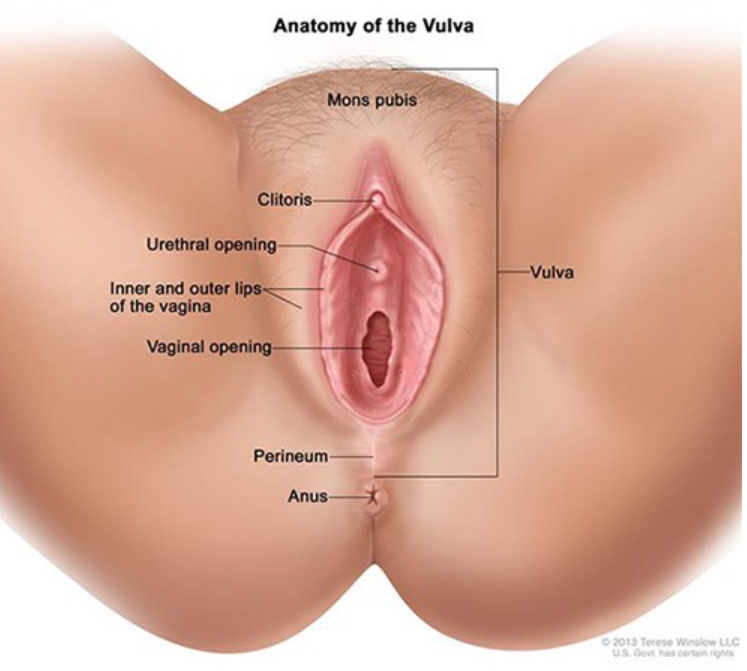
The gynecologic surgeon will insert a speculum into the vagina to allow visualization of the cervix, the opening of your uterus located at the back of the vagina.
Once the speculum is in place and the cervix visualized, the surgeon inserts a device called a uterine manipulator into the cavity of the uterus. This step facilitates the surgeon’s ability to safely operate and avoid injury to surrounding tissue such as the bladder, rectum, intestines, and ureter.
The surgeon will mark the surgical sites with a small marking pin. A small camera is inserted through an incision into the belly button. Air inflates and distends the abdomen to allow visualization of the pelvis. Three or four secondary ports are placed to allow the robotic arms to function.
The robot is then positioned over the body and attached to the ports. The laparoscopic camera is positioned to show the pelvic anatomy. Small instruments are passed through the additional ports. Scissors are attached to one robotic arm and a grasping device in the other. This allows the surgeon to operate with both hands.
The surgeon then moves away from the patient to the surgical consult to control the robot.
As the surgeon takes her seat, she adjusts the camera and robotic arms’ position to begin the surgery.
Many surgeons recommend complete removal of the fallopian tubes (bilateral salpingectomy) at the time of surgery as this technique reduces the risk of ovarian cancer.
The fallopian tubes are located and grasped with one instrument. Using the other hand, the surgeon clamps and cuts the tubes away from the adjacent anatomy.
The surgeon travels down the sides of the uterus freeing it from the connecting tissues. The round ligament and utero-ovarian ligaments are clamped, cauterized, and then cut. At each step, the surgeon will take precautions to control and avoid bleeding.
Towards to lower end of the uterus lies important anatomy. The surgeon will separate the bladder from the lower uterine segment to allow visualization of the cervix.
The surgeon will focus attention on the uterine arteries. These two blood vessels are the main blood supply to the uterus and travel over the ureters, which are the tubes connecting the kidney to the bladder.
Once the uterine arteries are controlled, the surgeon can safely separate the uterus from the vagina.
The surgeon makes a circular incision just below the cervix freeing the uterus. The uterus is delivered through the vagina and sent to the pathologist to analyze the tissue.
The surgeon then sews the edges of the vagina closed to form the vaginal cuff.
The surgeon examines all of the surgical sites for bleeding. When safe, the Obgyn removes the operative ports and sews the surgical incisions closed.
Once the procedure is complete, the surgical team completes a post-procedure review. All instruments and equipment are counted and verified. When finished, the anesthesiologist will begin to wake the patient up for transfer to the recovery room.


Once the patient enters the operating room, a series of safety steps must occur. This process takes about 20 minutes.
The operative time for robotic hysterectomy varies. The surgeon’s experience, surgical technique, patient body type, uterine size, and patient’s previous surgeries are all factors.
In general, patients should expect 1–2 hours of total operative time.
Postoperative recovery time will vary from person to person. Some surgeons will recommend an outpatient procedure while others prefer an overnight stay. The patients underlying health status, surgical complexity, and physician preference are all factors.
To be able to go home, each patient must meet specific discharge criteria. The patient’s vital signs must be stable. The patient must be alert, oriented, and able to walk with assistance. Postoperative nausea, vomiting, and pain must be controlled as well as confirmation of no postoperative bleeding.
The nursing team will go over discharge instructions, and the plan for postoperative pain management options will be confirmed.
Most women should be able to return to normal daily activities within a few weeks of surgery. The nursing team will help patients walk and move around a few hours after surgery to reduce blood clots’ risk, improve lung function, and expedite bowel function return.
Most patients will require pain medication like NSAIDs and narcotics for a time. Many experience discomfort in the right shoulder due to air irritating the nerves of the diaphragm.
Light bleeding, spotting, and brown or black discharge is common and expected. Sanitary napkins are safe to use.
You should speak with your physician regarding the resumption of exercise and sexual activity. Most can return to basic activities in one to two weeks. Sexual activity is typically restricted for 6–8 weeks to allow the vaginal cuff to heal.
Your doctor will schedule a postoperative examination 1–2 weeks after the procedure to evaluate the incisions.
You should call your doctor if you experience heavy vaginal bleeding, fevers, severe nausea or vomiting, worsening abdominal pain, or the inability to pass gas.
If you experience heavy bleeding, abdominal or pelvic pain, a fever, or pain that increases over 24 hours, call your physician. After any surgery, contact your physician if you meet any of the following criteria:
Robotic procedures require very little postoperative care. Keep the incisions clean and dry. Sexual activity should be avoided until cleared by your doctor. One may resume a normal diet the day of surgery and begin light exercise the day after the procedure or when you feel ready.
It is very important to provide your doctor with an updated list of all medications, vitamins, and dietary supplements prior to surgery. All medication and food allergies should be reviewed. Share any lab work, radiologic procedures, or other medical tests done by other healthcare providers with your surgeon prior to your procedure.
Source: https://medium.com/beingwell/robotic-hysterectomy-what-you-need-to-know-and-how-to-prepare-148d0201f80b
Quilting Angels Fidget Quilts have donated over 6000 masks to the DFW area. Read more
Understand morning sickness and what to do about it. Read more
An OB-GYN answers questions and explains best practices. Read more
Stigmatizing coronavirus infection inhibits society’s ability to stop the spread. Read more
Here are things you can do to reduce your discomfort. Read more
How to fix odor “down there”.
Let’s face it. Humans sometimes stink. Our genitals, butts, and armpits do not always smell like roses. Women expect postworkout smelly armpits, but no one is happy when the pungent odor comes from the vagina.
So, what causes the “not so fresh” feeling?
Sweat, food intake, medications, and hormonal changes all alter vaginal scent, but the most common cause of an unpleasant vaginal odor is an overgrowth of normal vaginal bacteria called bacterial vaginosis.
Bacterial vaginosis is easy to treat with antibiotics, but the crucial step is to confirm the diagnosis with a medical provider. Self-diagnosing often leads to errors. The malodorous situation “down there” will not improve if we are not treating the right thing.
While most women will get bacterial vaginosis at some point in their life, everyone wants to know why BV happens and how to get rid of it.
Bacterial vaginosis (BV) is not an infection in the traditional sense, but rather a condition caused by an overgrowth of anaerobic bacteria living in the vagina.
Vaginal bacteria are supposed to be present. Bacteria live on our skin, mouths, and gastrointestinal tracts all the time. These healthy bacteria help keep our body systems running smoothly. The vagina always contains small amounts of healthy, protective bacteria.
Vaginal bacteria and yeast live in perfect harmony, maintaining the vaginal ecosystem. Bacteria and yeast work to keep the vaginal chemistry pH balanced in the healthy range between 3.5–5.5.
Periodically, something disruptive happens to break the chemical balance allowing bacteria to flourish. When bacteria outgrows the counterbalancing yeast, women develop bacterial vaginosis.
When vaginal bacteria overpower and suppress yeast, women will notice a gray or yellow, fishy smelling discharge.
BV is the most common vaginal condition, and any woman can get it. BV is more common in sexually active women, but it is not a sexually transmitted infection.
BV is most common in ages 15 to 44, but it can happen at any age and in women who do not have sex.
The risk of bacterial vaginosis increases with:
BV symptoms vary from person to person. While some may have no symptoms, others will notice a fishy vaginal odor, vulvar irritation, or discomfort with urination. Some experience a watery or foamy white, yellow, or gray vaginal discharge.
These symptoms are often confused with STIs and vaginal yeast infections. Seeing your doctor or practitioner is the only way to determine if you have a BV and not a more severe problem.
The signs and symptoms of a BV are similar to other more serious infections. Trichomoniasis is a common STI that also causes itching and vaginal odor.
If left untreated, STIs and BV raise your risk of getting other STIs, including HIV. Untreated gonorrhea and chlamydia can lead to problems getting pregnant. BV can also lead to problems during pregnancy, such as preterm labor and premature delivery.
A doctor will do a pelvic exam to look for the characteristic discharge. The doctor may also use a cotton swab to take a sample of the discharge from the vagina.
A test can be done to see if the pH is elevated. The providers may add a chemical called KOH to perform a Whiff test. (Yes, this involves smelling the discharge). Finally, the provider may look at the sample under a microscope to evaluate for a particular finding called clue cells.
Nucleic acid amplification microbial testing is a widely available rapid test technology to help distinguish between yeast, bacterial vaginosis, and trichomoniasis.
BV is treated with prescription antibiotics. Metronidazole pills or vaginal gel are the most common. Clindamycin is a common acceptable alternative.
Sex partners do not need to be treated.
Patients suffering from recurrent bacterial vaginosis may qualify for more robust treatment protocols.
Many times, BV will resolve on its own. Vaginas are very effective at self-correcting. Untreated BV increases the risk of getting HIV, genital herpes, gonorrhea, chlamydia, and pelvic inflammatory disease. Women with HIV who get BV are also more likely to pass HIV to a male sexual partner.
The medicine used to treat BV is safe for pregnant women at any stage of pregnancy. All pregnant women with symptoms of BV should be tested and treated. Some evidence indicates a link between BV and preterm birth.
Researchers do not know exactly what causes BV, but we know ways to help the vagina maintain a normal pH and reduce the risk of BV. Steps include:
Thank you Sexography for publishing this article on Medium. Article originally published on Medika Life.
Blog Author: Dr. Jeff Livingston
Main Blog Photo By: Giulio_Fornasar stock by Getty
