Every day, patients ask if starting GLP-1 medications, like Semaglutide, means a lifelong commitment. The question is understandable. Long-term commitments are scary. But answering the question is putting the cart before the horse. We don’t have to decide what to do long-term when we have not achieved our immediate goal.
Before a patient has reached their ideal body weight or desired health goals, our focus should be on the journey, the here and now, and the hard work ahead to get the body of our dreams. When we look at weight loss through this lens, we realize that the journey isn’t only about reaching the goal but also about building habits to sustain that goal. Let’s dive into what we know about GLP-1 medications and how they fit into long-term weight management.
Understanding GLP-1 Medications and Their Effects
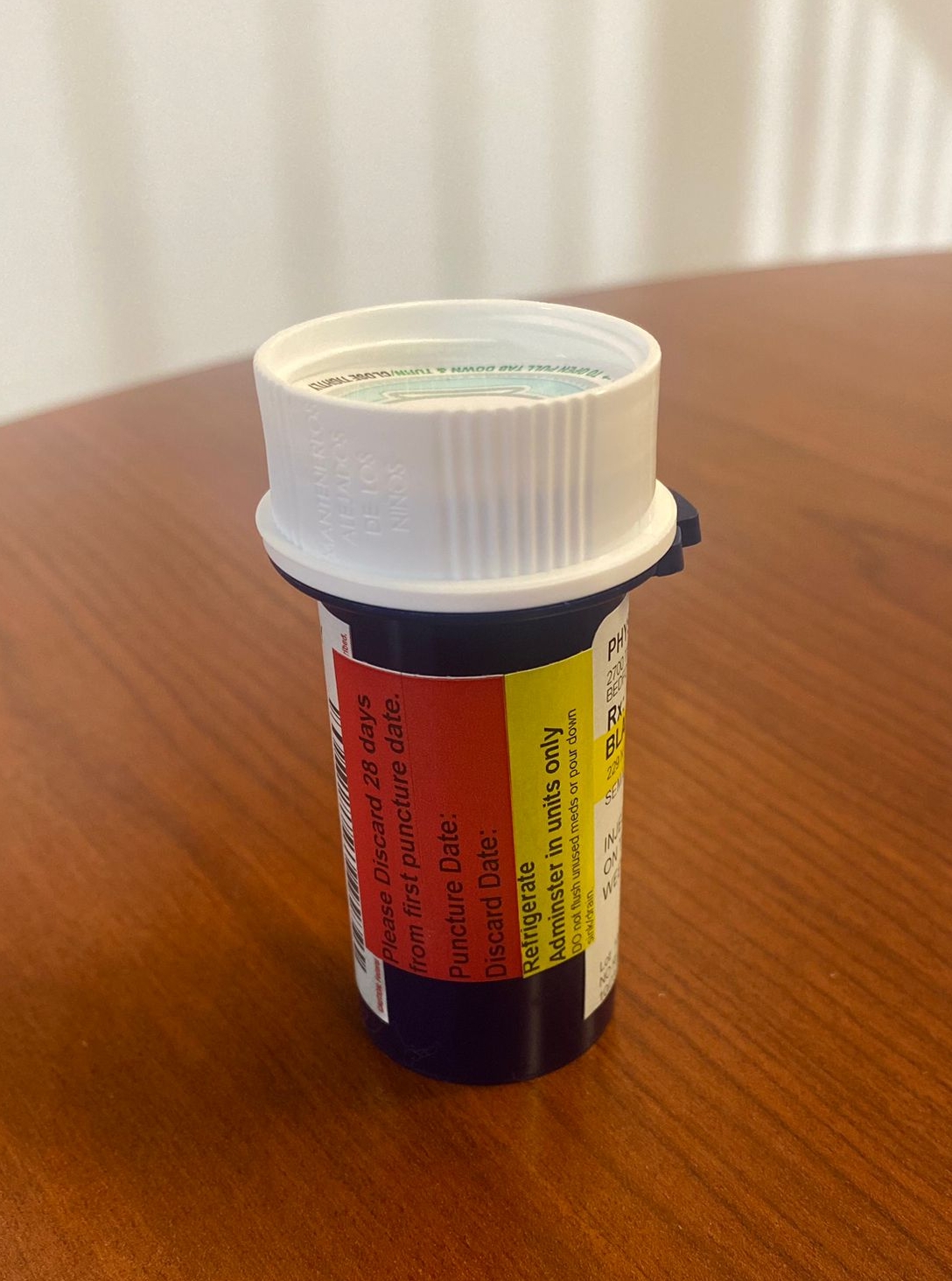
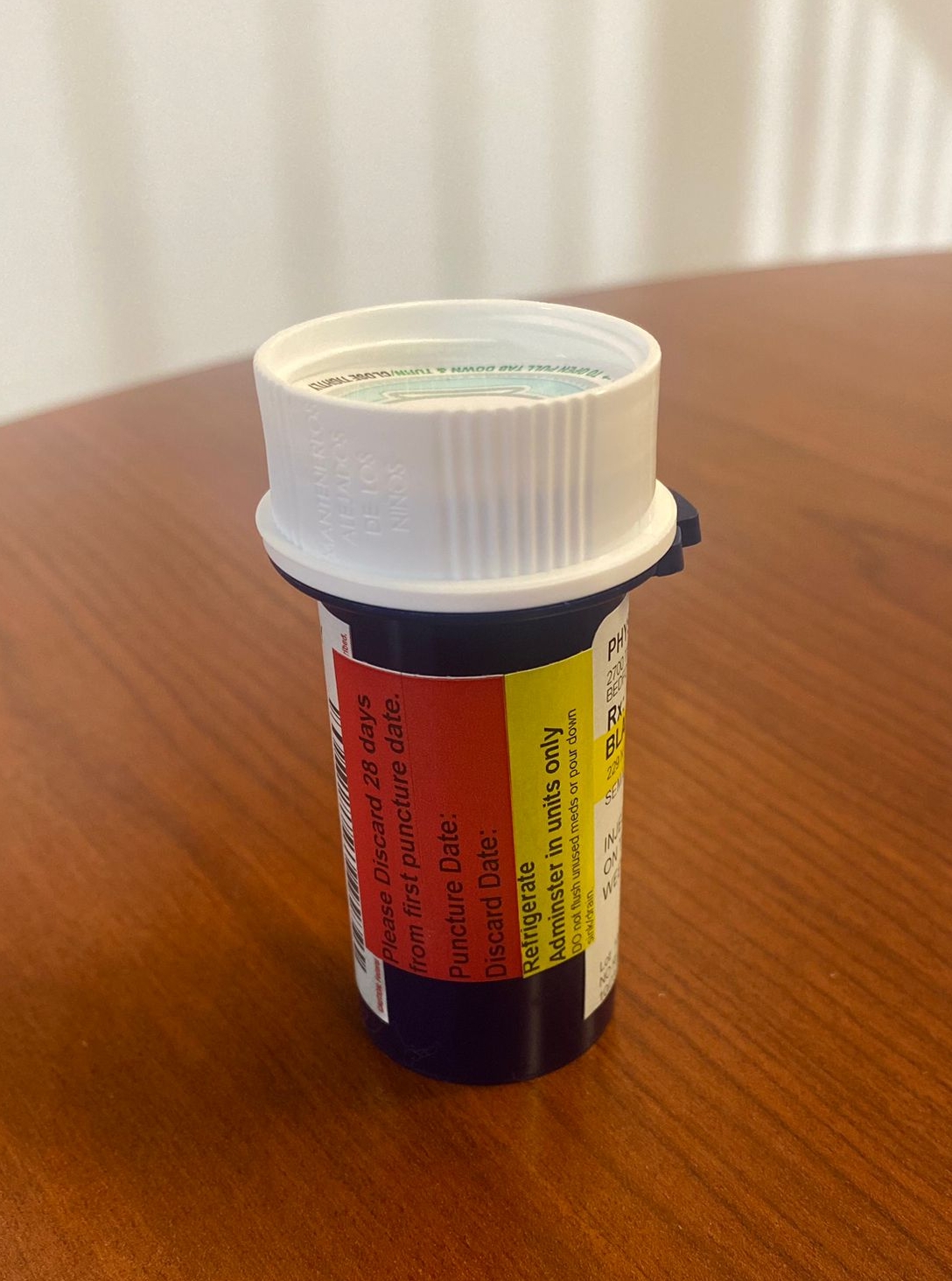
Photo by MacArthur Medical Center
- GLP-1 medications, such as Semaglutide, have revolutionized weight loss by helping patients control appetite. These medications work by triggering areas in the brain associated with satiety, effectively reducing our desire to overeat.
- GLP-1 medications don’t change who we are or our relationship with food but help to make the process a bit easier. Stopping medication doesn’t “cause” weight gain, but our appetite will no longer be suppressed. Think of it like removing a training wheel: without that support, some may find it more challenging to stay balanced with appetite control.
- When we stop taking GLP-1 medication, we are removing the training wheel. Our appetite will return to its natural state. Weight gain can and will return unless we have made sustainable changes to our eating and lifestyle.
The Role of Lifestyle in Sustaining Weight Loss
- Our weight loss program emphasizes the importance of viewing GLP-1 medications as one tool in our toolbelt. Our approach integrates nutrition, exercise, and lifestyle modifications to encourage sustainable habits that outlast medication.
- GLP-1 medications aren’t shortcuts or end-all solutions; they’re part of a broader strategy to reach a healthier weight and a better quality of life.
- We hope that by the time patients reach their goal, they’ll adopt a healthier lifestyle that naturally sustains their weight.
- When a patient is ready to transition off medication, they’ll have a foundation in place that keeps them on track, even if their appetite increases.

Photo by Dr Jeff Livingston
Long-Term Options for Weight Maintenance
Every patient’s weight journey is unique, and for some, maintenance involves a small, ongoing dose to help keep appetite in check. These maintenance doses aren’t meant to continue weight loss but to maintain a steady, controlled appetite. Some patients prefer this as a way to stay accountable, while others may feel ready to stop altogether.
Additionally, there’s growing interest in the anti-aging and anti-inflammatory potential of GLP-1 medications, though research is still ongoing. For some, staying on a minimal dose offers other health benefits beyond weight control.
Conclusion: It’s About Choices, Not Obligations
When we look at weight loss through this lens, we realize that the journey isn’t only about reaching the goal but also about building habits to sustain that goal.
The decision to stay on or eventually taper off GLP-1 medications should be based on personal goals, lifestyle, and health needs. The best approach aligns with the individual’s journey and provides flexibility. Remember, weight loss is a journey with many stages; each person’s path is unique.
Blog Author: Dr. Jeff Livingston
Main Blog Photo By: Getty Images on Unsplash

 No one was listening to my excuses.
No one was listening to my excuses.