Phexxi; Have You Heard About the New Hormone-Free Contraceptive?
Phexxi is a new on-demand, nonhormonal, option for women. Read more
Phexxi is a new on-demand, nonhormonal, option for women. Read more
How to fix odor “down there”.
Let’s face it. Humans sometimes stink. Our genitals, butts, and armpits do not always smell like roses. Women expect postworkout smelly armpits, but no one is happy when the pungent odor comes from the vagina.
So, what causes the “not so fresh” feeling?
Sweat, food intake, medications, and hormonal changes all alter vaginal scent, but the most common cause of an unpleasant vaginal odor is an overgrowth of normal vaginal bacteria called bacterial vaginosis.
Bacterial vaginosis is easy to treat with antibiotics, but the crucial step is to confirm the diagnosis with a medical provider. Self-diagnosing often leads to errors. The malodorous situation “down there” will not improve if we are not treating the right thing.
While most women will get bacterial vaginosis at some point in their life, everyone wants to know why BV happens and how to get rid of it.
Bacterial vaginosis (BV) is not an infection in the traditional sense, but rather a condition caused by an overgrowth of anaerobic bacteria living in the vagina.
Vaginal bacteria are supposed to be present. Bacteria live on our skin, mouths, and gastrointestinal tracts all the time. These healthy bacteria help keep our body systems running smoothly. The vagina always contains small amounts of healthy, protective bacteria.
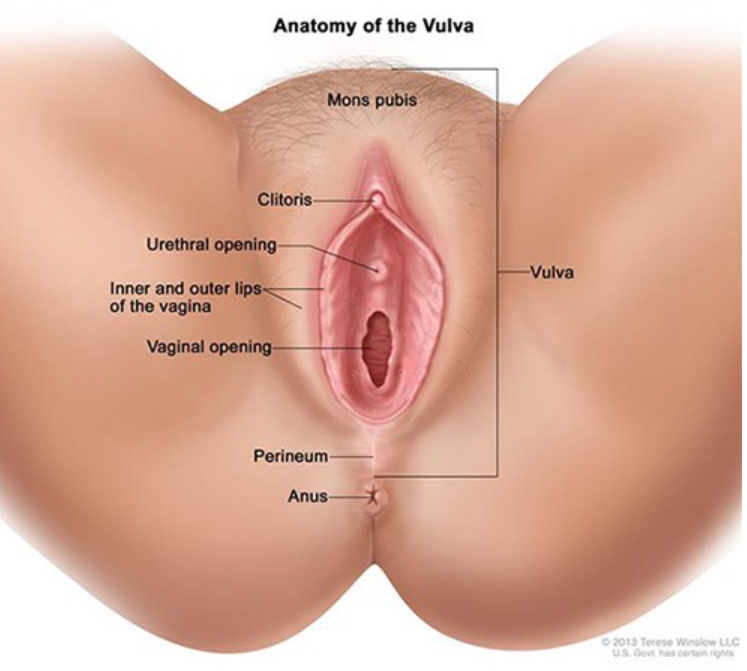
Vaginal bacteria and yeast live in perfect harmony, maintaining the vaginal ecosystem. Bacteria and yeast work to keep the vaginal chemistry pH balanced in the healthy range between 3.5–5.5.
Periodically, something disruptive happens to break the chemical balance allowing bacteria to flourish. When bacteria outgrows the counterbalancing yeast, women develop bacterial vaginosis.
When vaginal bacteria overpower and suppress yeast, women will notice a gray or yellow, fishy smelling discharge.
BV is the most common vaginal condition, and any woman can get it. BV is more common in sexually active women, but it is not a sexually transmitted infection.
BV is most common in ages 15 to 44, but it can happen at any age and in women who do not have sex.
The risk of bacterial vaginosis increases with:
BV symptoms vary from person to person. While some may have no symptoms, others will notice a fishy vaginal odor, vulvar irritation, or discomfort with urination. Some experience a watery or foamy white, yellow, or gray vaginal discharge.
These symptoms are often confused with STIs and vaginal yeast infections. Seeing your doctor or practitioner is the only way to determine if you have a BV and not a more severe problem.
The signs and symptoms of a BV are similar to other more serious infections. Trichomoniasis is a common STI that also causes itching and vaginal odor.
If left untreated, STIs and BV raise your risk of getting other STIs, including HIV. Untreated gonorrhea and chlamydia can lead to problems getting pregnant. BV can also lead to problems during pregnancy, such as preterm labor and premature delivery.
A doctor will do a pelvic exam to look for the characteristic discharge. The doctor may also use a cotton swab to take a sample of the discharge from the vagina.
A test can be done to see if the pH is elevated. The providers may add a chemical called KOH to perform a Whiff test. (Yes, this involves smelling the discharge). Finally, the provider may look at the sample under a microscope to evaluate for a particular finding called clue cells.
Nucleic acid amplification microbial testing is a widely available rapid test technology to help distinguish between yeast, bacterial vaginosis, and trichomoniasis.
BV is treated with prescription antibiotics. Metronidazole pills or vaginal gel are the most common. Clindamycin is a common acceptable alternative.
Sex partners do not need to be treated.
Patients suffering from recurrent bacterial vaginosis may qualify for more robust treatment protocols.
Many times, BV will resolve on its own. Vaginas are very effective at self-correcting. Untreated BV increases the risk of getting HIV, genital herpes, gonorrhea, chlamydia, and pelvic inflammatory disease. Women with HIV who get BV are also more likely to pass HIV to a male sexual partner.
The medicine used to treat BV is safe for pregnant women at any stage of pregnancy. All pregnant women with symptoms of BV should be tested and treated. Some evidence indicates a link between BV and preterm birth.
Researchers do not know exactly what causes BV, but we know ways to help the vagina maintain a normal pH and reduce the risk of BV. Steps include:
Thank you Sexography for publishing this article on Medium. Article originally published on Medika Life.
Blog Author: Dr. Jeff Livingston
Main Blog Photo By: Giulio_Fornasar stock by Getty
Understanding emergency contraception.
Dear politicians, health policymakers, reporters, and highly-opinionated social media friends. Plan B is not an abortion pill. Stop calling it that.
Plan B is the brand name of one form of emergency contraception. RU486 (Mifepristone) is a medication used to induce abortion. Plan B and RU486 are not the same medication. Emergency birth control prevents pregnancy. Abortion medication terminates a pregnancy.
Our views on abortion vary. We must understand what we are arguing about. Our country’s public policy and heated Facebook debates should at least be based on facts. Emergency contraception is completely different than a medical abortion. In fact, emergency contraception prevents the need for abortions while preventing unplanned pregnancy.
Emergency contraception (EC) contains progesterone, a hormone produced naturally by the ovaries. It is often called “the morning after” pill. Common brands, such as Plan B, are available over the counter without a prescription. EC is formulated with a high dose of progesterone. This hormonal blast disrupts, delays, or prevents ovulation. High dose progesterone also thickens the cervical mucus creating a toxic environment for sperm. It will not terminate an already established pregnancy.
Over-the-counter emergency birth control should be used within 72 hours of unprotected sex. Presciption EllaOne (ulipristal acetate) can be taken up to 5 days after unprotected sex. The earlier it is used, the better it works. EC decreases the risk of pregnancy by 70–80% (ACOG). It is not a great primary form of contraception. Emergency contraception is called Plan B and not Plan A for a reason.
Progesterone does not cause abortion. Emergency contraception decreases the risk of pregnancy by inhibiting ovulation. If conception has already, then it is too late for emergency contraception. Once pregnancy occurs, the ovary forms a type of ovary cyst called a corpus luteum. It produces progesterone to support the growing pregnancy. Taking emergency contraception will only add more progesterone to support the developing fetus.
Side effects include nausea, vomiting, headache, breast tenderness, abdominal pain, dizziness, and fatigue. Those side effects will subside within 1–2 days after treatment. Because EC disrupts ovulation, irregular bleeding is common. Users may experience menstrual changes, including spotting, heavy bleeding, or altered timing of the next menstrual period.
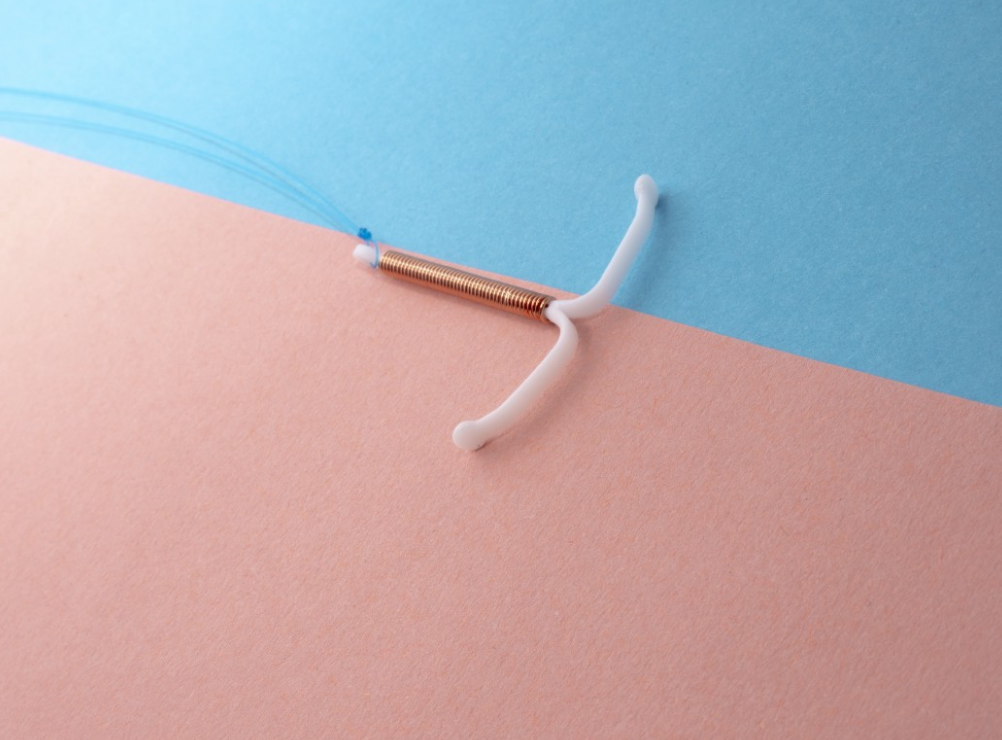
Photo by Reproductive Health Supplies Coalition on Unsplash
A copper intrauterine device (IUD) is the most effective form of emergency contraception. An IUD is a small T-shaped device inserted into the cavity of the uterus. It should be placed within 72 hours of unprotected intercourse. It prevents pregnancy by inhibiting sperm’s ability to swim towards the egg. It reduces the risk of pregnancy by 99% and provides effective birth control for up to ten years.
Emergency contraception is a safe option to prevent pregnancy after having sex without a condom or birth control. Other much more effective forms of contraception are available to help prevent pregnancy over the long term. Emergency contraception also does not protect against HIV or other sexually transmitted infections.
The abortion pill is a misnomer. Two medications, when combined, can terminate a pregnancy. RU486 (Mifepristone) competes with progesterone at the receptor sites. After taking RU486, a second medication called Misoprostol is given to induce uterine contractions. The combination of these two medications is used in abortion clinics for medical abortions. RU486 is highly regulated and only available under medical supervision at a clinic that offers abortion services.
Thank you Sexography for publishing this article on Medium.
Blog Author: Dr. Jeff Livingston
Blog Photo By: Alex Hockett on Unsplash