As an obstetrician, an important part of my job is preconceptional counseling. Making sure that hopeful mothers are healthy, eating right, and avoiding harmful behaviors and substances in preparation for pregnancy is a very important duty to me as their OB doctor. Counseling women before pregnancy has even occurred is always challenging though. It’s hard for people to keep themselves healthy for something that hasn’t even happened yet. However, certain topics are so beneficial and universal to all women that they cannot be ignored. Folic acid supplementation and the prevention of neural tube defects is one such topic. So, what is folic acid and why is it so important?
Folic acid is a B vitamin that is essential for numerous bodily functions. Folic acid is crucial for production of DNA, which is the genetic code for all cells in your body. Therefore, it is important for rapid cell division and times of growth such as during infancy or pregnancy. It also plays a vital role in the formation of red blood cells which carry oxygen throughout your body and therefore prevents you from becoming anemic (low red blood cell count). Unfortunately, folic acid is not a vitamin that your own body produces so you must get it from your diet.
So, how is folic acid helpful to pregnant women specifically? Overwhelming evidence has shown that folic acid reduces your baby’s risk of neural tube defects (NTDs). What are neural tube defects? They are defects (openings) in the baby’s spine or brain that cause varying degrees of disability or even death. Normally the neural tube closes very early at approximately the fourth week of gestation. When it does not close completely or at all, a neural tube defect occurs. Because of this it is very important for women to have adequate folic acid intake prior to and during early pregnancy. In fact, taking adequate amounts of folic acid reduces the chance of NTDs by up to 70%!
Here are some common questions I often get asked by patients regarding folic acid:
How can I get enough folic acid?
There are two ways to get folic acid in your body:
- Take a vitamin that has folic acid in it. This is easy. Just ask your doctor to write a prescription for prenatal vitamins for you. You can also get them over the counter in grocery stores, pharmacies, and even discount stores. They are inexpensive and can be purchased without a prescription. Most bottles with 100 vitamins only cost ~$5, which is only 5 cents per vitamin! You buy them just as you would any other grocery item. Just be sure that the label says 100% of the daily value of folic acid which is 400 mcg – the recommended daily dose.
- Eat foods that have folic acid in them. The most common and convenient food is breakfast cereal although other foods are now fortified with folic acid as well. Fortification of cereals with folic acid occurred in 1996 and was done primarily to prevent NTDs. One bowl of cereal each morning usually provides sufficient amounts of folic acid, although with foods, you can never be completely sure that you are getting the recommended amounts because it all depends on how much you take in.
How much folic acid should I be taking? When should I start?
With vitamins, it’s always hard to remember the recommended doses and timing because they all differ depending on who you ask. Luckily, when it comes to folic acid, all recommendations are essentially the same. You should be taking 400 mcg (micrograms) of folic acid every day starting at least 1 month prior to pregnancy and continuing it at least through the first trimester. Waiting to start folic acid until you find out you are pregnant is too late. Most women will not even know they are pregnant until 8-10 weeks after conception which is 1-2 months after the neural tube has already formed and thus too late to prevent these birth defects. In fact, almost half of all pregnancies are unplanned! For these two reasons, it is important for every woman of childbearing age to be on folic acid even if not planning to become pregnant.
Should I ever be on a higher dose of folic acid?
With all rules there are exceptions, and folic acid is no different. There are two main instances where a higher dose of folic acid is necessary. If you, your partner, or your child has had a neural tube defect you should be on a much higher dose. The recommended dose is 4 mg (milligrams) or 4000 mcg (10 times the normal dose discussed above). You will need a special prescription for this from your doctor. Taking multiple doses of prenatal or multivitamins may lead to dangerously high amounts of other vitamins in your body. Similarly, if you have a history of seizures and are on anti-epileptic medications, you should be on 4 mg of folic acid as some seizure medications can lead to an increased risk of NTDs. Again, this increased dose should be started at least 1 month prior to conception and continued at least through the first trimester.
What other foods have folic acid in them?
Lots of foods now have folic acid in them since food fortification has been in place for almost 20 years now. These include breakfast cereals, breads, rice, pasta, and other grain products. The best natural sources of folic acid are green leafy vegetables like spinach, turnip greens, and collard greens. Other foods rich in folic acid include other vegetables (broccoli, asparagus, carrots, squash), citrus fruits, seeds, nuts, peas, and beans. By eating these foods, a woman can be confident that she is getting folic acid in her everyday diet. This however should not be a replacement but rather a supplement to your daily vitamin.
What if I have trouble remembering to take a vitamin each day?
Women are busy these days, no doubt about it! Between kids, jobs, groceries, and errands, it’s hard to set aside time each day to take a vitamin. We just sometimes flat out forget as well. But just as regular exercise, adequate sleep, and healthy eating are important to your health, taking folic acid is too. Try and coordinate taking a vitamin each day with your daily routine activities (i.e. brushing your teeth, showering, putting on your makeup). Or try coordinating with someone else like your child or spouse who is also taking a daily vitamin so you can keep each other in check. Keep the bottle in sight next to your bathroom sink or on the kitchen counter so that you will be frequently reminded of it. Also, with smartphones these days, it’s easy to set a daily alarm or reminder. These are just a few ways to help you remember. Do whatever is most comfortable and convenient for you.
What if I can’t swallow pills?
Nowadays, multivitamins with folic acid come in various shapes and sizes. Many pills are chewable or in liquid form. Some even have fruity or chocolate flavors to make them more tolerable to those who have trouble with a pill’s bad taste.
Neural tube defects are the second most common class of birth defects second only to congenital heart defects in babies. However, NTDs are one of the only birth defects in which primary prevention is possible. Therefore, it is vital to make sure that all women are aware of this simple measure to prevent a birth defect that could negatively impact your baby’s life.


 These are very common non-cancerous tissue growths in the uterus. The size and number of these fibroids is variable… can be a single fibroid or multiple fibroids, and can range from very small to the size of a cantaloupe. They can be found on a stalk inside or outside the uterus. They can also be found in any layer of the uterus: in the muscle wall (intramural), under the outer layer (subserosal), or just below the inner lining of the uterus (submucosal).
These are very common non-cancerous tissue growths in the uterus. The size and number of these fibroids is variable… can be a single fibroid or multiple fibroids, and can range from very small to the size of a cantaloupe. They can be found on a stalk inside or outside the uterus. They can also be found in any layer of the uterus: in the muscle wall (intramural), under the outer layer (subserosal), or just below the inner lining of the uterus (submucosal).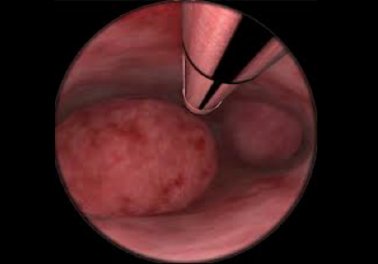 These are small protrusions of the uterine lining (endometrium) that grow, become fragile, and start to bleed. Here is a picture of two polyps and the Symphion device.
These are small protrusions of the uterine lining (endometrium) that grow, become fragile, and start to bleed. Here is a picture of two polyps and the Symphion device.
